The intricate relationship between the gut and the brain has long fascinated scientists, but recent breakthroughs in understanding the gut-brain axis have opened new frontiers in neuroscience. Among the most compelling discoveries is the role of gut microbiota in neurodegenerative diseases, particularly Parkinson’s disease (PD). Once considered a disorder confined to the brain, PD is now increasingly viewed as a systemic condition with roots in the gastrointestinal tract. This paradigm shift is reshaping how researchers approach diagnosis, treatment, and even prevention.
The Gut-Brain Connection: A Two-Way Street
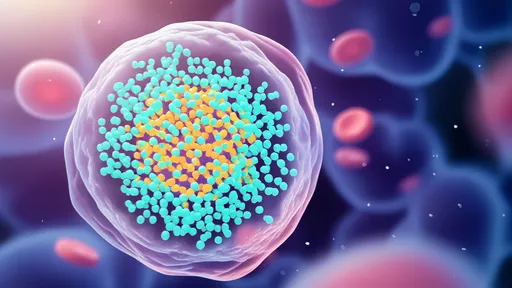
The gut and brain communicate through a complex network of neural, hormonal, and immunological pathways. The vagus nerve, often dubbed the "gut-brain superhighway," plays a pivotal role in this dialogue. But perhaps the most surprising player in this relationship is the gut microbiome—the trillions of bacteria, viruses, and fungi residing in our intestines. These microbes don’t just aid digestion; they produce neurotransmitters, modulate inflammation, and even influence the blood-brain barrier. Disruptions in this delicate ecosystem, known as dysbiosis, have been linked to a range of neurological disorders, including PD.
Parkinson’s Disease: A Gut-First Pathology?
Emerging evidence suggests that Parkinson’s might begin in the gut years before motor symptoms appear. Pathological hallmarks of PD, such as alpha-synuclein aggregates, have been found in the enteric nervous system (the "second brain" in the gut) of patients decades before clinical diagnosis. Some researchers propose that misfolded alpha-synuclein may travel from the gut to the brain via the vagus nerve, seeding pathology in vulnerable regions. This "prion-like" spread could explain why gastrointestinal symptoms like constipation often precede motor dysfunction by years.
Microbial Fingerprints of Parkinson’s
Metagenomic studies have identified distinct microbial signatures in PD patients. Reduced levels of anti-inflammatory butyrate-producing bacteria (e.g., Faecalibacterium prausnitzii) and increased populations of pro-inflammatory microbes (e.g., Enterobacteriaceae) are common findings. These shifts may contribute to intestinal permeability ("leaky gut"), systemic inflammation, and ultimately, neuroinflammation. Intriguingly, some gut microbes can produce amyloid proteins or metabolize levodopa—potentially influencing both disease progression and treatment efficacy.
Therapeutic Horizons: From Probiotics to Fecal Transplants
The gut microbiome represents a promising therapeutic target for PD. Early-stage clinical trials are exploring interventions like precision probiotics, prebiotic fibers, and fecal microbiota transplantation (FMT). A 2022 pilot study found that FMT from healthy donors improved motor and non-motor symptoms in PD patients, possibly by restoring microbial balance and reducing inflammation. Meanwhile, dietary strategies like the Mediterranean diet—rich in polyphenols and fiber—may nurture beneficial microbes while suppressing harmful ones.
Challenges and Future Directions
Despite exciting progress, significant hurdles remain. The gut microbiome is highly individualized, influenced by genetics, diet, antibiotics, and geography. Establishing causal relationships—rather than mere associations—between specific microbes and PD requires longitudinal studies and animal models. Researchers are also developing microbial biomarkers for early detection, potentially enabling interventions before irreversible neuronal damage occurs.
The exploration of the gut-brain axis in Parkinson’s disease exemplifies how viewing neurological disorders through a systemic lens can yield transformative insights. As this field matures, it may not only revolutionize treatment but also challenge our fundamental understanding of where—and how—neurodegenerative diseases begin.

By /Jul 2, 2025

By /Jul 2, 2025
By /Jul 2, 2025
By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025
By /Jul 2, 2025

By /Jul 2, 2025

By /Jul 2, 2025
By /Jul 2, 2025

By /Jul 2, 2025
By /Jul 2, 2025